Mad cow disease, scientifically known as bovine spongiform encephalopathy (BSE), is a rare and fatal neurological disorder that primarily affects cattle. Its human counterpart, variant Creutzfeldt-Jakob disease (vCJD), has been a significant concern due to its potential transmission through the consumption of contaminated beef products. While cases of vCJD are extremely rare, understanding the disease and how to protect yourself remains essential.
In this article, we’ll delve into the origins and causes of this disease, how it can affect humans and the strategies in place to minimize risks.
What is Mad Cow Disease?
Mad cow disease, formally known as BSE, is a rare and fatal neurological disorder in cattle. The name “spongiform” refers to the sponge-like appearance of the brain tissue in affected animals, where tiny holes form as a result of the disease.
What Causes Disease?
The underlying cause of BSE is prions, which are misfolded proteins. Unlike viruses or bacteria, prions lack genetic material but are still infectious. These abnormal prions trigger healthy proteins in the brain to misfold, leading to an accumulation of damaged proteins. This disrupts normal brain function, resulting in severe neurological damage and eventually death.
Why is BSE a Concern for Humans?
While BSE primarily affects cattle, its link to variant Creutzfeldt-Jakob disease in humans has heightened public awareness. vCJD, a type of prion disease, is believed to be transmitted through the consumption of beef products contaminated with prions from infected cattle. First identified during a mad cow disease outbreak in the United Kingdom in the 1980s, the disease raised global concerns and led to widespread reforms in livestock farming and food safety.
How Do Humans Get Mad Cow Disease?
The human variant of mad cow disease, variant Creutzfeldt-Jakob disease, is an exceptionally rare condition. Understanding its transmission is critical for reducing risks and implementing safety measures.
How Do Humans Get Prion Disease?
The primary method of transmission is through the consumption of beef products contaminated with prions. These prions are abnormal proteins found in the central nervous system tissues (such as the brain and spinal cord) of cattle infected with BSE. Unlike bacteria or viruses, prions are extremely resistant to heat, so standard cooking does not destroy them.

Other forms of prion disease that are unrelated to beef consumption include:
- Sporadic CJD: The most common form, occurring randomly without a known cause.
- Familial CJD: A rare genetic condition caused by inherited mutations.
- Iatrogenic CJD: Acquired through medical procedures, such as the use of contaminated surgical instruments or tissues, though stringent sterilization methods have made this exceedingly rare.
Can Vcjd Spread Through Blood Transfusions?
There have been a few documented cases suggesting vCJD transmission via blood transfusions from infected donors. As a precaution, many countries now restrict blood donations from individuals who lived in areas heavily affected by BSE outbreaks during certain periods.
Food Safety Measures
In response to the BSE crisis, robust regulations have been implemented to ensure the safety of the food supply. These include:
- Removal of high-risk materials: Brain, spinal cord, and other tissues most likely to harbor prions are excluded from human food.
- Bans on feeding practices: The use of ruminant-derived protein in cattle feed has been prohibited to prevent the spread of BSE.
- Increased surveillance: Routine testing of cattle and monitoring of slaughterhouse practices have been established worldwide.
These measures have significantly reduced the likelihood of BSE-contaminated beef entering the food chain, making the risk of vCJD in humans extremely low.
Recognizing the Symptoms of Mad Cow Disease in Humans
Variant Creutzfeldt-Jakob disease is the human form of mad cow disease and is both progressive and fatal. Recognizing its symptoms early is vital for diagnosis and supportive care, although the early signs can often resemble other conditions.

Early-Stage Symptoms
The initial signs of vCJD are predominantly psychiatric and can often lead to misdiagnoses. These early symptoms may include:
- Depression: Persistent feelings of sadness and disinterest in usual activities.
- Anxiety: Excessive fear or nervousness.
- Irritability: Increased levels of agitation or frustration.
- Insomnia: Difficulty sleeping or staying asleep.
- Social Withdrawal: Avoidance of friends and family interactions.
- Psychosis: In rare cases, individuals may experience hallucinations or delusions.
Later Stage Symptoms
As vCJD progresses, neurological issues become more severe and debilitating:
- Cognitive Decline: Difficulty with memory, focus, and logical reasoning.
- Coordination Issues: Problems with balance and motor skills, often resulting in frequent falls.
- Involuntary Movements: Uncontrollable jerking, muscle spasms, or tremors.
- Speech Impairments: Slurred speech or trouble forming sentences.
- Vision Problems: Blurred vision or other visual disturbances.
- Severe Dementia: Rapid cognitive deterioration, leading to an inability to perform daily tasks.
How Do Symptoms Progress?
The symptoms of vCJD worsen over a period of months, culminating in significant physical and mental decline. Most individuals succumb to the disease within a year of symptom onset, often falling into a coma during the final stages.
Important Note
Although vCJD presents with serious and recognizable symptoms, it is extremely rare. Experiencing any of these signs does not mean you have vCJD. If you’re concerned about neurological symptoms, consulting a healthcare professional is essential for an accurate diagnosis and peace of mind. Mad Cow Disease Outbreaks: A Look at the Past
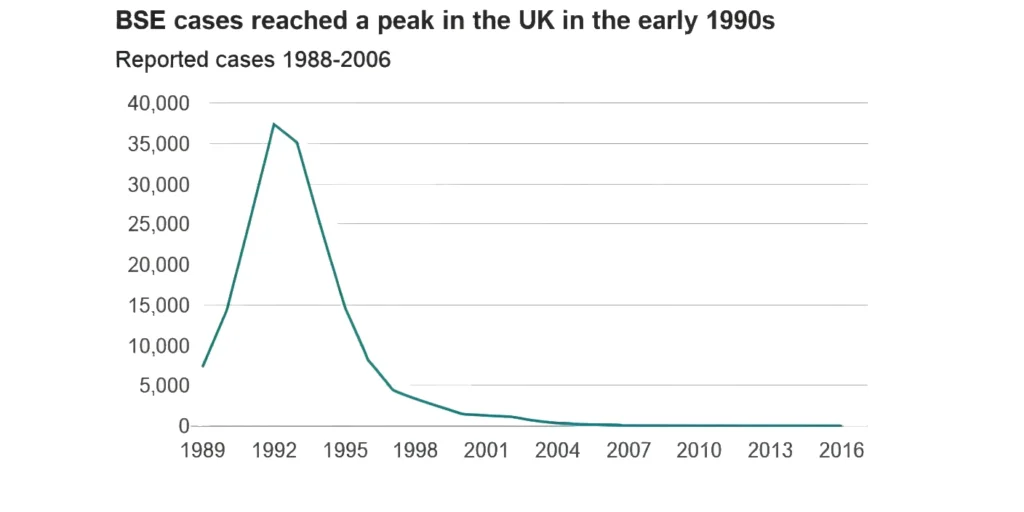
Though mad cow disease is rare today, its emergence in the late 20th century had a significant impact on global public health and food safety practices. The most notable outbreak occurred in the United Kingdom, beginning in the mid-1980s and peaking during the early 1990s. This outbreak was traced back to the use of meat-and-bone meal in cattle feed, which included tissues from infected animals.
Lessons Learned from Outbreaks
The UK outbreak and smaller incidents in other countries prompted the development of stringent measures to prevent the spread of Bovine Spongiform Encephalopathy and its human variant:
- Ban on Meat-and-Bone Meal in Cattle Feed: This practice, identified as the main cause of the UK outbreak, is now widely prohibited.
- Removal of Specified Risk Materials: High-risk tissues, such as the brain and spinal cord, are systematically removed from the food chain to minimize potential exposure to infectious prions.
- Surveillance Programs: Countries worldwide have implemented strict monitoring systems to detect BSE in cattle populations and ensure food safety.
Current Risk of Mad Cow Disease
Today, the risk of contracting variant Creutzfeldt-Jakob disease through beef consumption is extremely low, thanks to the rigorous control measures established after the outbreaks. While vigilance remains essential, the global food industry has successfully reduced the threat posed by mad cow disease. These efforts provide consumers with much greater confidence in the safety of beef products.
Prevention and Treatment
While there is no cure for vCJD, significant measures have been taken to reduce the risk of transmission. Here’s what you need to know about prevention strategies and current treatment options.

How to Avoid Getting Mad Cow Disease?
The risk of contracting mad cow disease in humans is now extremely low due to stringent global food safety regulations. To further minimize your risk:
- Choose Beef from Reputable Sources: Opt for products from countries with strict BSE surveillance and control programs.
- Avoid High-Risk Tissues: Refrain from consuming brain, spinal cord, or other nervous system tissues from cattle, as these are most likely to harbor prions if the animal is infected.
- Stay Cautious When Traveling: In regions with a history of BSE outbreaks, inquire about the origin of beef and the safety protocols in place.
- Stay Informed: Regularly check updates from reliable health organizations like the CDC and WHO for the latest information on prion diseases and food safety measures.
Can Mad Cow Disease Be Cured?
Unfortunately, no cure currently exists for vCJD or other prion diseases. Once symptoms develop, the condition is invariably fatal. Treatment focuses on:
- Symptom Management: Medications may be used to alleviate pain, control psychiatric symptoms, or reduce muscle spasms.
- Supportive Care: This involves providing comfort and maintaining the patient’s quality of life through physical therapy, nutritional support, and other interventions.
Promising Research Directions
Despite the lack of a cure, ongoing research aims to better understand prion diseases and develop potential treatments. Areas of exploration include:
- Preventing Prion Formation: Investigating compounds that might inhibit the conversion of normal proteins into prions.
- Clearing Prions from the Brain: Exploring treatments to neutralize or remove existing prions from affected tissues.
While these efforts are still in their early stages, advances in prion research offer hope for future therapies. Until then, prevention remains the most effective strategy for combating mad cow disease and its human variant.
Addressing Common Concerns
Mad cow disease, though exceedingly rare, sparks concern due to its severe implications and unusual characteristics. Below are answers to some of the most frequently asked questions:
Why Are Prions So Scary?
Prions are a unique and alarming type of infectious agent because:
- Resilience to Sterilization: Prions are resistant to standard methods used to inactivate bacteria and viruses. Cooking, radiation, and many disinfectants do not destroy them.
- Long Incubation Period: Prion diseases can take years or even decades to manifest symptoms after exposure, making it difficult to identify and respond to the source of infection.
- Devastating Impact: Once prions affect the brain, they cause a chain reaction that leads to progressive and irreversible damage. There are currently no cures or effective treatments.
This combination of factors makes prions uniquely challenging to manage from both a public health and research perspective.
Is Cow Brain Safe to Eat?
No, consuming cow brain or other nervous system tissues from cattle is not considered safe, especially in regions with a history of mad cow disease outbreaks. These tissues are the most likely to carry infectious prions if the animal is infected.
- Regulatory Safeguards: Many countries, including the US, have banned the use of “specified risk materials” (brain, spinal cord, and other nervous tissues) in both human food and animal feed to minimize risk.
- Best Practice: Avoid eating these parts entirely, even if sourced from regions with robust food safety practices, as the potential risk is not worth it.
Important Takeaway
Due to enhanced safety measures, the likelihood of contracting vCJD from beef is extremely low today. However, awareness of food safety regulations and cautious dietary choices remain essential for reducing risks further. When in doubt, opt for beef from trusted sources and avoid high-risk tissues altogether.
Conclusion
Mad cow disease and its human counterpart, variant Creutzfeldt-Jakob disease are grave conditions but exceedingly rare. Global implementation of strict food safety regulations has drastically reduced the risk of transmission, making the likelihood of contracting disease minimal.
Understanding the disease, including its transmission routes and prevention measures, empowers individuals to make safer dietary choices. Sourcing beef from reputable suppliers, avoiding high-risk tissues like the brain and spinal cord, and staying updated through trusted organizations like the CDC and WHO can further minimize potential risks.
By prioritizing food safety and remaining informed, you can confidently enjoy a balanced diet while safeguarding your health.
Frequently Asked Questions (FAQs)
Can you get mad cow disease from eating muscle meat (steaks, roasts)?
The risk of contracting vCJD from consuming muscle meat like steaks or roasts is extremely low. Infectious prions are primarily concentrated in tissues like the brain and spinal cord, not in muscle meat.
How long does it take to show symptoms of vCJD after exposure?
The incubation period for disease is unusually long, often spanning years or even decades. This means that individuals can carry the abnormal prions for a significant amount of time before symptoms emerge.
Is mad cow disease still a threat today?
Thanks to strict regulatory measures and surveillance programs, the risk of mad cow disease has been significantly reduced. However, continued vigilance by public health authorities is necessary to maintain these low levels of risk.
Are there any diagnostic tests?
Currently, there is no definitive test for diagnosing vCJD in living individuals. Diagnosis is typically based on clinical symptoms, neurological examinations, brain scans, and cerebrospinal fluid tests. A brain biopsy conducted post-mortem is required to confirm the diagnosis conclusively.






