When the body becomes unnaturally rigid, with arms and legs extended straight, and the head arching backward, it signifies more than just a muscle reaction—it’s a critical neurological warning. Decerebrate posture is an involuntary physical response that typically indicates severe damage to the brainstem. This condition often results from traumatic brain injuries, strokes, or other serious medical events like cerebral edema. It reflects a breakdown in the communication pathways between the brain and spinal cord, making it a key indicator of severe neurological disruption.
In this guide, we will examine the causes of decerebrate posturing, how it differs from related neurological signs such as decorticate posturing, and why urgent medical care is essential. We’ll also explore its implications for recovery and outline the diagnostic and management approaches used by healthcare professionals.
What Is a Decerebrate Posture?
Decerebrate posture is an abnormal, rigid bodily stance resulting from severe neurological damage. It is defined by extensor rigidity, where the arms and legs extend outward in a stiffened, hyperextended position. The elbows and knees become locked, the wrists and fingers flex inward, and the head may arch backward. This posture is entirely involuntary, occurring due to disrupted neural communication between the brainstem and spinal cord.
The presence of this reflex is a critical indicator of damage to the brainstem, specifically the midbrain and pons. These areas play a vital role in controlling muscle tone and voluntary movements. Common causes include traumatic brain injuries, intracranial hemorrhages, or conditions such as cerebral hypoxia, where the brain experiences insufficient oxygen levels.
Decorticate vs. Decerebrate Posturing: Understanding the Difference
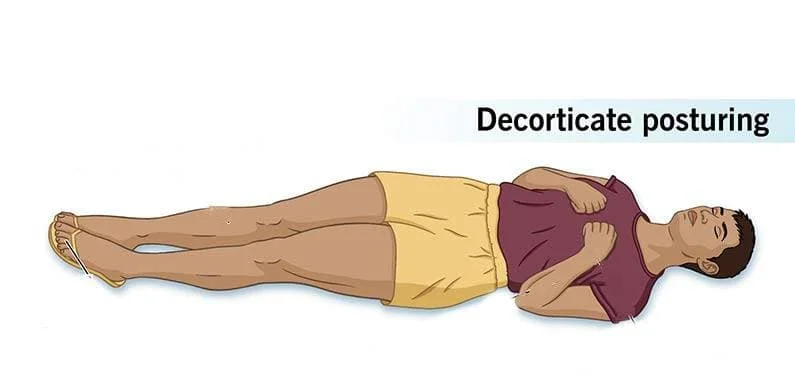
Both decorticate and decerebrate posturing signal severe neurological injury, but their presentation and the brain regions involved differ significantly. Differentiating between these abnormal postures is critical for accurate diagnosis and management.
What is the difference between decorticate and decerebrate posturing?
- Appearance: Arms flexed at the elbows and wrists, held tightly against the chest. Legs extended and internally rotated.
- Cause: Indicates damage to structures above the brainstem, such as the cerebral hemispheres, internal capsule or thalamus.
- Appearance: Arms extended and rotated inward at the sides, wrists flexed, and fingers clenched. Legs rigidly extended with feet pointing downward.
- Cause: Reflects more severe damage involving the brainstem, specifically the midbrain or pons.
Key Difference:
- Decorticate Posturing involves flexion of the upper limbs and extension of the lower limbs, pointing to damage higher in the brain.
- Decerebrate Posture involves extension of both upper and lower limbs, indicating deeper, more severe brainstem injury.
This distinction offers critical clues about the location and extent of brain damage, aiding healthcare professionals in tailoring appropriate interventions.
Causes of Decerebrate Posturing
Decerebrate postures indicates severe brainstem damage and requires immediate medical attention. Below are the primary causes of this condition, presented in a reader-friendly format:
- Traumatic Brain Injury (TBI):
Severe head trauma from car accidents, falls, or other injuries can damage the brainstem, leading to decerebrate. - Stroke:
Strokes affecting the brainstem disrupt blood flow and oxygen supply, which can result in neurological dysfunction and abnormal posturing. - Brain Tumors:
Tumors in or near the brainstem exert pressure on surrounding tissues, potentially damaging critical areas and causing posturing. - Hypoxia:
Lack of oxygen to the brain, caused by cardiac arrest, drowning, or severe respiratory issues, can damage the brainstem and trigger this posture. - Infections:
Severe infections such as encephalitis (brain inflammation) or meningitis (inflammation of brain and spinal cord membranes) can lead to brain swelling. - Metabolic Disorders:
Rare conditions like hepatic encephalopathy (caused by liver failure) or severe hypoglycemia (low blood sugar) can impair brain function and cause this reflex.
Important Note:
Decerebrate posture is a critical medical emergency. Immediate intervention is essential to identify the underlying cause and provide life-saving treatment.
Recognizing the Symptoms: What to Look For
Decerebrate posturing is characterized by distinct physical signs, indicating a critical neurological emergency. Here are the key symptoms to watch for:
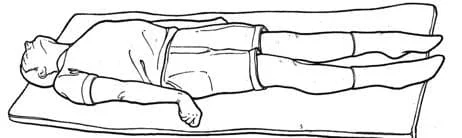
- Rigidly Extended Limbs: Both arms and legs straighten outward and lock in a stiff, hyperextended position.
- Arched Back and Neck (Opisthotonus): The spine and head curve backward, creating a noticeable arch.
- Clenched Teeth and Jaw: The jaw may tighten, often accompanied by teeth grinding or locking.
- Flexed Wrists and Fingers: Hands may curl inward, with fingers bent tightly toward the palms.
These physical manifestations are often accompanied by altered consciousness, such as confusion or coma, underscoring the severity of the situation.
Diagnosis and the Glasgow Coma Scale (GCS)
Decerebrate posture is identified through a detailed clinical evaluation, focusing on the patient’s physical state and responsiveness to external stimuli. Physicians assess for rigid limb extension, arched posture, and reactions to pain or other stimuli. Following these exams, advanced imaging techniques, such as CT scans or MRIs, are often used to determine the precise location and cause of the brainstem injury or bleeding.
What Is the Glasgow Coma Scale (GCS)?
The Glasgow Coma Scale (GCS) is a standardized 15-point tool used to evaluate consciousness levels in patients with brain injuries. It measures three key responses:
- Eye Response (1-4): From no response (1) to spontaneous eye-opening (4).
- Verbal Response (1-5): From no verbal sounds (1) to clear, coherent speech (5).
- Motor Response (1-6): From no movement (1) to obeying commands (6).
This scale provides a structured method for determining the severity of brain injury and guiding treatment priorities.
What Is the GCS Score for Decerebrate Posturing?
A GCS motor score of 2 is assigned to decerebrate postures, categorized as “abnormal extension.” This score indicates severe brain dysfunction, typically placing the patient’s overall GCS score at 8 or below, a range classified as coma.
What Does a GCS Between 9 and 12 Indicate for a Patient?
A GCS score of 9–12 reflects moderate brain injury. Patients within this range may:
- Drift between states of consciousness.
- Exhibit confused verbal responses or disorientation.
- React purposefully to painful stimuli but not consistently obey commands.
While this score indicates a serious condition, it often suggests a better prognosis compared to scores of 8 or below.
Key Takeaway:
The GCS motor score of 2 associated with decerebrate posturing signals critical brainstem damage, requiring urgent medical intervention. A GCS of 9–12, though serious, offers a greater chance of recovery with prompt and effective treatment.
Differential Diagnosis of Decerebrate Posturing
Decerebrate posture is a critical indicator of severe neurological dysfunction, but other conditions can mimic its presentation. Accurate diagnosis is essential to identify the root cause and initiate appropriate treatment.
What Is the Differential Diagnosis?
Several neurological and medical conditions can produce symptoms or postures that resemble decerebrate posturing. These include:
- Decorticate Posturing: Unlike decerebrate, decorticate involves arm flexion and leg extension. Distinguishing between the two can help localize brain damage.
- Severe Hypoglycemia: Critically low blood sugar levels may sometimes cause posturing that appears similar to decerebrate rigidity.
- Opisthotonos: Extreme hyperextension and spasticity seen in conditions like tetanus, meningitis, or strychnine poisoning can mimic posturing.
- Seizures: Certain seizure types may involve abnormal body movements or positions that could be confused.
- Dystonic Reactions: Adverse effects of certain medications can cause sudden, involuntary muscle contractions (dystonia), producing abnormal postures.
The Diagnostic Process:
To differentiate decerebrate postures from other conditions, physicians rely on a systematic approach:
- Neurological Examination: Assessing muscle tone, reflexes, and responsiveness to stimuli.
- Medical History: Understanding the context, such as recent head trauma or medication use.
- Imaging Tests: CT or MRI scans to identify brain injuries or abnormalities.
- Blood Tests: Checking for metabolic imbalances, such as hypoglycemia or toxin exposure.
- Observation of Accompanying Symptoms: Evaluating fever, seizure activity, or signs of infection.
Key Takeaway:
Differentiating decerebrate posturing from other conditions is vital for accurate diagnosis and effective intervention. A comprehensive evaluation, combining clinical observations and diagnostic tools, helps pinpoint the cause and guide treatment strategies.
Treatment and Prognosis
Decerebrate posture is a serious neurological symptom, not a standalone condition. Its treatment focuses on identifying and addressing the underlying cause, whether it be a traumatic brain injury, stroke, brain tumor or another life-threatening condition. There is no direct cure for the posturing itself; instead, medical efforts aim to stabilize the patient and manage the root issue.
Treatment Approach
- Addressing the Underlying Cause:
The primary objective is diagnosing and treating the condition causing decerebrate posturing. Depending on the cause, treatment may include:- Surgery: For brain injuries, tumors, or bleeding.
- Medications: To reduce swelling (e.g., corticosteroids), control seizures, or manage infections.
- Therapeutic Interventions: For strokes or metabolic imbalances.
- Supportive Care:
Patients with decerebrate postures typically require close monitoring in an intensive care unit (ICU). Key supportive measures include:- Airway and Oxygenation: Ensuring a clear airway and providing supplemental oxygen or mechanical ventilation if needed.
- Hemodynamic Support: Managing blood pressure to ensure adequate brain perfusion.
- Temperature Regulation: Preventing hyperthermia or hypothermia.
- Infection Control: Using antibiotics for infections such as meningitis.
- Nutritional Support: Providing proper nutrition through enteral or parenteral feeding methods.
- Physical Therapy: Preventing muscle contractures and maintaining joint mobility.
What Is the Outcome of Decerebrate Posturing?
The prognosis for decerebrate posturing largely depends on the cause and extent of the brain damage:
- Poor Prognosis Indicators: Its often signals severe brainstem injury or dysfunction, which is associated with a high risk of mortality or long-term disability.
- Recovery Possibilities: Early and aggressive treatment of the underlying cause may improve outcomes. Some individuals regain partial neurological function if the damage is not extensive.
- Long-Term Outcomes: Many patients who survive may experience:
- Permanent neurological deficits, including cognitive and physical impairments.
- Persistent vegetative states in severe cases.
- In rare situations, substantial recovery, depending on the reversibility of the initial injury.
Key Takeaway:
Its indicates a critical medical emergency requiring immediate intervention. While the prognosis is often grim, timely and targeted treatment can improve survival rates and offer some patients a chance for partial recovery.
Frequently Asked Questions (FAQs)
Can it be reversed?
The reversibility of decerebrate posturing largely depends on the underlying cause and the extent of brain damage. In cases where prompt and effective treatment addresses the root issue, such as reducing brain swelling or treating an infection, improvement may occur. However, if the damage to the brainstem is severe or irreversible, the posturing may persist permanently.
How long can someone live with this condition?
Survival time after exhibiting decerebrate postures varies widely. Factors such as the underlying cause, the extent of brain injury, and the quality of medical care play critical roles. Some individuals may live for weeks, months, or even years with significant neurological impairments, while others may succumb to their condition quickly if the damage is extensive.
Is it painful?
Determining pain levels in patients is challenging because they are typically unresponsive or have a severely altered level of consciousness. While the posture itself may not cause pain, the underlying conditions triggering it—such as trauma, swelling, or infections—can be painful. Effective pain management is an integral part of the supportive care provided to these patients.
Can you recover from decorticate posturing?
Compared to decerebrate, decorticate posturing generally indicates less severe brain damage, offering a more favorable prognosis. Recovery is possible, especially with early intervention, but the outcome depends on the severity of the initial injury and the effectiveness of treatment. Some patients regain significant function, while others may experience lasting neurological deficits.
What is it a sign of?
Decerebrate posturing is a clear indication of severe brain damage, particularly involving the brainstem. It signifies a critical disruption in the neural pathways that control voluntary movement and muscle tone. Common causes include traumatic brain injuries, strokes, brain tumors, and conditions like hypoxia or brain infections.
How is it treated?
Treatment for decerebrate postures focuses on resolving the underlying cause. For example:
- Stroke-related posturing: May involve clot-dissolving medications or surgery to reduce brain pressure.
- Trauma-induced posturing: Requires immediate intervention to stabilize the patient, reduce swelling, or perform neurosurgery.
- Infections: Treated with antibiotics or antivirals as needed.
Supportive care is also critical and may include mechanical ventilation, nutritional support, and therapies to manage secondary complications such as infections or seizures.