Post menstrual syndrome — sometimes called after-period symptoms — refers to the physical and emotional changes some people experience shortly after their period ends. While PMS (premenstrual syndrome) is widely known, this post-period phase gets far less attention, despite being just as real for many.
If you’ve ever wondered, “Why do I still feel off after my period?” — with symptoms like fatigue, cramps, mood swings, or anxiety lingering past the last day of bleeding — you’re not alone. In this guide, we’ll break down what post menstrual syndrome is, when it starts, how long it can last, what symptoms to look for, and how to manage them effectively through self-care and professional help.
What Is Post Menstrual Syndrome?
Post menstrual syndrome is a term used to describe a set of physical and emotional symptoms that appear after your menstrual period ends — not before, like in PMS. While it’s less widely discussed, many people report feeling off, tired, or emotionally overwhelmed in the days following their period.
These after-period symptoms can include:
- Mood swings and irritability
- Fatigue or low energy
- Headaches or cramps
- Anxiety, brain fog, or restlessness
Unlike PMS, which occurs in the luteal phase before bleeding begins, post menstrual syndrome happens just after menstruation stops, as the body shifts into the follicular phase of the cycle. Hormones like estrogen and testosterone begin to rise again, and for some, this transition can trigger uncomfortable symptoms.
When Does Post Menstrual Syndrome Start?
Symptoms typically begin right after menstrual bleeding ends, usually within 1 to 3 days. For some, they may even overlap with the final days of menstruation. This phase marks the start of the follicular phase, when hormone levels are still low but beginning to rise.
That shift — especially if ovulation is delayed or skipped — can lead to unexpected physical and emotional reactions. Unlike PMS, which builds up before menstruation, post menstrual syndrome starts after the period has ended, making it distinct in both timing and hormonal context.
Post Menstrual Syndrome vs. PMS: What’s the Difference?
Though both involve hormonal shifts and similar symptoms, post menstrual syndrome and premenstrual syndrome (PMS) occur at different times in the cycle.
| Key Difference | PMS | Post Menstrual Syndrome |
| Timing | 1–2 weeks before period | 1–7 days after period ends |
| Hormonal context | Estrogen/progesterone drop | Estrogen/testosterone rebound |
| Symptoms | Bloating, cravings, sadness | Fatigue, anxiety, mood swings |
| Commonness | Very common (up to 90%) | Less studied, but real for many |
In short: PMS happens before your period, post menstrual syndrome happens after. And while the medical community is still studying the latter, those who experience it know it’s more than just an afterthought.
Post Menstrual Syndrome Symptoms
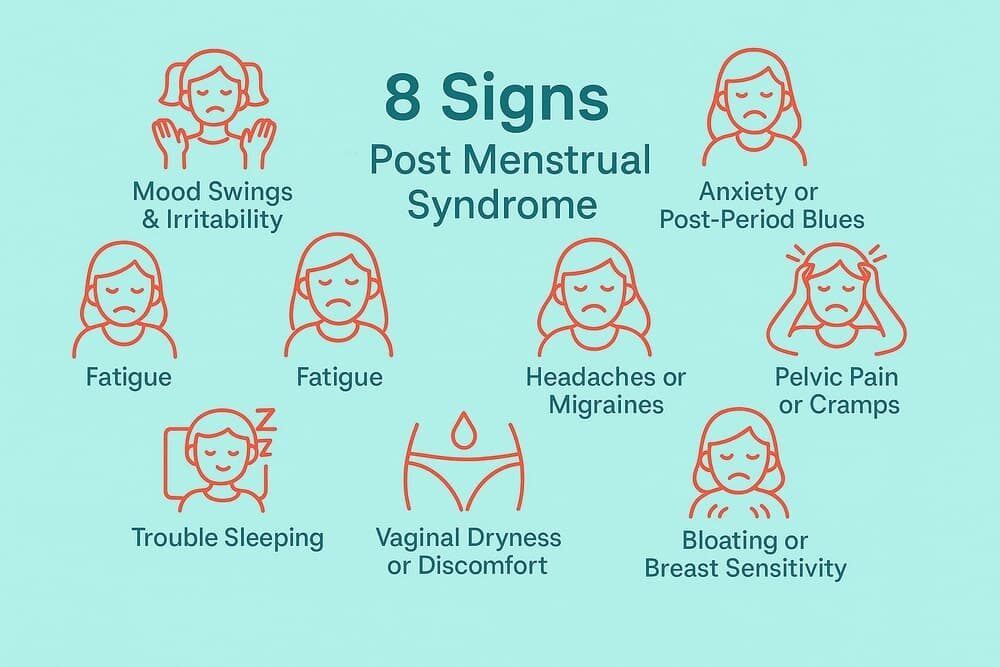
Post menstrual syndrome symptoms can affect both your body and mind — often mimicking PMS, but showing up after your period ends. While research is still catching up, many people report feeling “off” in the days following menstruation.
Below are some of the most commonly reported after-period symptoms:
1. Mood Swings & Irritability
Sudden emotional shifts, irritability, or feeling uncharacteristically sensitive or tearful. These mood changes are often described as more intense than typical PMS by some individuals.
2. Anxiety or Post-Period Blues
Feelings of anxiety, nervousness, or low mood that emerge after bleeding ends. Some people also experience restlessness, mental fog, or even mild depression during this phase.
3. Fatigue
Lingering tiredness that doesn’t match your usual post-period energy rebound. You may feel physically drained for a few days, despite expecting to feel “back to normal.”
4. Headaches or Migraines
Hormonal shifts can trigger tension headaches or migraines even after menstruation ends — similar to those seen during PMS but with a delayed onset.
5. Pelvic Pain or Cramps
Some report lingering cramps or discomfort in the lower abdomen after bleeding has stopped. There may also be back, neck, or joint pain — and in some cases, pain during intercourse.
⚠️ If pain is severe or persistent, consult a healthcare provider to rule out underlying conditions like endometriosis.
6. Vaginal Dryness or Discomfort
Mild burning, itching, or dryness in the days following menstruation. This can affect comfort and may lead to discomfort during sex.
7. Trouble Sleeping
Difficulty falling asleep or waking frequently — often linked to anxiety, hormonal changes, or physical discomfort in the post-period phase.
8. Bloating or Breast Sensitivity
While less common than during PMS, some people still experience bloating or mild breast tenderness post-period due to hormonal fluctuations.
✍️ Quick Note on Variability
Not everyone will experience all of these symptoms, and severity can vary from cycle to cycle. Emotional symptoms like mood swings and anxiety tend to be the most commonly reported.
🧠 According to Healthline, people have reported symptoms such as anxiety, mood shifts, headaches, and even physical discomfort like joint pain in the days after their period — supporting the idea that this is a real, trackable pattern for many.
What Causes Post Menstrual Syndrome?

Post menstrual syndrome is not yet a formally recognized medical condition, which means the exact cause remains uncertain. However, many experts believe that hormonal fluctuations after your period are the most likely trigger — especially in the first days of the new cycle.
Here are the most common science-backed theories behind what causes post menstrual syndrome:
1. Hormonal Imbalance After Period
As your period ends, your body enters the follicular phase of the menstrual cycle. Hormones like estrogen and testosterone begin to rise again — sometimes sharply. This shift can trigger emotional and physical symptoms.
🧬 Dr. Soma Mandal explains that a surge of estrogen and testosterone after menstruation may explain many post-period symptoms. Especially in cycles without ovulation (anovulatory cycles), hormone levels can become erratic.
2. Hormone Withdrawal Effects
Another theory suggests your body is reacting to the sudden drop in progesterone and estrogen that happens right before and during your period. This “withdrawal” effect may linger into the days after bleeding ends — causing PMS-like symptoms even though menstruation has stopped.
3. Underlying Health Conditions
Hormonal imbalances can also result from conditions like:
- PCOS (Polycystic Ovary Syndrome)
- Insulin resistance
- Thyroid disorders
These can affect ovulation and hormone regulation — potentially worsening post menstrual syndrome symptoms. Hormonal birth control may also influence the severity and pattern of symptoms depending on the formulation.
4. Blood Sugar Fluctuations & Diet
High intake of sugar or refined carbs can cause blood sugar spikes and oxidative stress, which may throw off hormonal balance. This can worsen mood swings, fatigue, or bloating in the days after your period.
5. Stress & Lifestyle Factors
Stress, poor sleep, and lack of nutrients make your body more vulnerable to hormonal instability. If your lifestyle is already stretched thin, your system might struggle more to “bounce back” after menstruation ends.
🧪 What Science Says
While these are the leading theories, more research is needed to fully understand the causes of post menstrual syndrome. That said, your symptoms are real — and many doctors now recognize post-period distress as a valid experience.
📌 According to research cited by the National Institutes of Health (NIH), current studies show no consistent relationship between hormonal levels and depressive symptoms across the menstrual cycle. While some women do report mood changes in the follicular phase (the time after menstruation), large-scale studies suggest that individual variation plays a significant role. This means that post-period symptoms like anxiety or low mood may not stem from universal hormonal shifts — but rather from how each person’s body responds to those changes.
How Long Does Post Menstrual Syndrome Last?
If you’re wondering how long post menstrual syndrome symptoms last, the answer is: typically just a few days after your period ends. However, the duration can vary from person to person.
🗓️ Typical Duration
Most people report that symptoms such as fatigue, mood swings, or bloating fade within:
- 1 to 3 days after menstruation
- Occasionally, up to 7 days in moderate cases
- Rarely, as long as 10–14 days, especially if there’s an underlying hormonal imbalance or skipped ovulation.
How long does post menstrual syndrome last?
Usually just a few days after your period, but symptoms can occasionally last up to 2 weeks.
🔄 Why It Varies
The duration depends on several factors:
- Hormonal rebound speed: Some bodies recalibrate hormones quickly, others take longer.
- Presence of health conditions: PCOS, thyroid issues, or insulin resistance may prolong symptoms.
- Lifestyle factors: High stress, poor sleep, and nutritional imbalances may make recovery slower.
If your symptoms last more than 14 days after your period ends, it’s a good idea to check with your doctor to rule out other possible causes.
📌 Tip: Tracking your symptoms each cycle can help identify patterns and provide helpful information for your healthcare provider.
Impact on Daily Life & When to Seek Help
Even though post menstrual syndrome isn’t officially recognized in medical literature, its effects are very real — and they can take a toll on your quality of life.
🌥 How It Affects Your Day-to-Day
Post menstrual symptoms like fatigue, irritability, and pain can interfere with your ability to function normally:
- Struggling to concentrate at work or school
- Feeling emotionally drained in relationships
- Losing motivation to exercise or socialize
- Experiencing low mood or anxiety for no clear reason
These aren’t “just in your head.” Many people feel out of sync for several days after their period — and that deserves attention and care.
📊 Is Post Menstrual Syndrome Common?
While up to 90% of menstruating people experience premenstrual symptoms, post-period symptoms are less frequently reported. According to anecdotal evidence from health professionals, roughly 10% of individuals may experience noticeable symptoms after their period.
That means:
You’re not alone — but it’s also normal if others around you don’t relate. This may be why even some doctors are unfamiliar with the pattern at first.
🩺 When Should You See a Doctor?
If your symptoms feel too intense or don’t go away, it’s important to seek medical advice — even if the term “post menstrual syndrome” isn’t an official diagnosis.
You should consider seeing a doctor if:
✅ Symptoms persist beyond 10–14 days after your period ends
✅ You experience debilitating pain, deep mood changes, or signs of depression
✅ Your symptoms interfere with daily life, work, or relationships
✅ You’re unsure if it’s hormonal, or possibly linked to another condition like thyroid imbalance, PCOS, or anxiety disorders
Doctors can rule out underlying issues, suggest blood tests, or recommend treatments like hormone therapy or mood support.
💡 Pro Tip: Keep a symptom diary. Tracking when and how symptoms show up can help your doctor better understand the pattern — and give you more tailored support.
How to Manage and Relieve Post Menstrual Syndrome Symptoms

If you’re dealing with fatigue, mood swings, or cramps after your period, you’re not alone. While post menstrual syndrome isn’t a formally recognized medical condition, its symptoms are real — and there are several ways to manage them.
🧘 Lifestyle Remedies That Help
Small changes to your routine can offer noticeable relief. Try these evidence-informed, self-care strategies:
1. Reduce stress daily
Chronic stress can amplify hormonal fluctuations. Relaxation techniques such as yoga, mindfulness, or even a walk in nature can regulate mood swings and ease physical tension.
2. Prioritize quality sleep
Lack of sleep can worsen irritability and fatigue. Aim for 7–9 hours of restful sleep, stick to a regular sleep schedule, and avoid screens before bed.
3. Move your body gently
Low-impact exercise like walking, swimming, or stretching boosts endorphins and reduces aches. You don’t need to hit the gym — just stay lightly active.
4. Eat for hormone balance
A nutrient-rich diet supports mood and energy. Focus on fiber, omega-3 fats, and magnesium-rich foods (leafy greens, avocado, seeds). Limit added sugar, caffeine, and ultra-processed snacks.
5. Consider helpful supplements
Talk to a doctor about iron (especially if you had heavy bleeding), B-complex vitamins, magnesium, or vitamin E — all linked to energy and mood regulation.
6. Hydrate and rest
Water helps fight bloating and headaches. Listen to your body — if you’re tired, don’t push it. A warm bath, a heating pad, or a short nap can go a long way.
💊 Medical Treatments
If lifestyle changes aren’t enough, professional help can offer additional relief:
- Over-the-counter meds: Pain relievers like ibuprofen or naproxen can ease cramps and headaches.
- Hormonal therapy: Some people benefit from birth control pills or IUDs to smooth hormone fluctuations. Always consult a gynecologist.
- Antidepressants or anti-anxiety medications: For severe mood symptoms, low-dose SSRIs may help. This should be evaluated by a psychiatrist or primary care provider.
- Therapy (CBT or counseling): Talking with a therapist helps you cope with anxiety, low mood, or emotional overwhelm — especially if these symptoms are recurrent.
- Treat underlying conditions: Hormonal imbalances from PCOS, thyroid issues, or insulin resistance might worsen symptoms. Testing and treatment can address root causes.
Managing post menstrual syndrome symptoms takes time and personalization. Some find relief through sleep and diet; others benefit from medical guidance. What matters most is tuning into your body — and knowing you’re not alone.
If symptoms persist or significantly disrupt daily life, talk to your doctor. You don’t need an official diagnosis to start feeling better.
Post Menstrual Syndrome or Pregnant? How to Tell the Difference
Feeling tired, bloated, or moody after your period — and wondering if it might mean you’re pregnant? You’re not alone. The line between post menstrual syndrome symptoms and early pregnancy signs can feel blurry. Here’s how to tell them apart with clarity.
🔁 Similarities That Can Confuse You
Some common symptoms overlap in both cases, including:
- Fatigue
- Mood swings
- Mild cramps or bloating
- Breast tenderness
That’s why it’s easy to question: Is this just hormonal fallout after my period — or something more?
Key Differences to Pay Attention To
Here’s how to differentiate between post menstrual syndrome or early pregnancy:
| Symptom Timing | Post Menstrual Syndrome | Early Pregnancy |
| Menstrual Cycle | Occurs after a normal period ends | You won’t have a real period |
| Symptom Onset | Begins right after bleeding stops | Starts around missed period time |
| Mood/Fatigue/Cramps | Yes | Yes |
| Nausea or Morning Sickness | Rare | Common |
| Breast/Nipple Changes | Mild tenderness | Darkening, swelling likely |
| Implantation Bleeding? | No (period is over) | Possible – lighter, shorter than normal bleeding |
🧪 Still Not Sure? Take a Pregnancy Test
If you’ve had a normal period, pregnancy is less likely — but not impossible. Hormonal fluctuations post-period can explain many symptoms. That said, the surest way to know is with a home pregnancy test taken after a missed period.
Testing around two weeks after ovulation provides accurate results. If your next period doesn’t arrive, test — and if symptoms persist or worsen, speak to a healthcare provider.
✅ Quick tip: If you’re tracking your cycle, note when symptoms start and whether your period was typical. This helps clarify patterns and improves your chances of early detection or accurate diagnosis.
Conclusion & Key Takeaways
Post menstrual syndrome may not be an official medical diagnosis, but the symptoms are real — and many people feel the effects in the days after their period ends.
Here’s what to remember:
- 💡 You’re not imagining it. Mood swings, fatigue, cramps, and anxiety after your period are real symptoms reported by many — even if they aren’t as widely recognized as PMS.
- ⏱️ It usually lasts a few days, but can stretch longer depending on hormone fluctuations, stress, or underlying conditions.
- 🌿 There are ways to manage it. Stress relief, sleep, gentle exercise, balanced nutrition, and self-care all play a role. In some cases, professional support or medical treatment may help.
- 📝 Tracking your symptoms — when they start, how long they last, and how intense they are — can help you spot patterns and guide conversations with your doctor.
- ❤️ You’re not alone. Understanding what’s happening in your body is empowering. With the right tools and support, you can feel more balanced — and take charge of your cycle, not just survive it.
FAQ
1. What is post menstrual syndrome, and how is it different from PMS?
Post menstrual syndrome includes symptoms that occur after your period ends, unlike PMS which happens before. While both can involve mood changes, cramps, and fatigue, the timing helps distinguish them.
2. When does post menstrual syndrome usually start and how long does it last?
Symptoms typically begin right after your period ends and may last for a few days to up to two weeks, depending on hormonal fluctuations and individual health.
3. What are the most common symptoms of post menstrual syndrome?
Symptoms can include fatigue, irritability, mood swings, anxiety, cramps, headaches, and even vaginal dryness or sleep issues in some cases.
4. Can post menstrual symptoms be a sign of early pregnancy?
Some symptoms overlap, like fatigue or breast tenderness, but post-period symptoms usually follow a normal period. If in doubt, a pregnancy test is the best next step.
5. What causes post menstrual syndrome?
Experts believe hormonal shifts after menstruation, especially changes in estrogen and progesterone levels, play a central role. Stress, diet, and underlying conditions may also contribute.
6. How can I manage or relieve post menstrual syndrome symptoms naturally?
Lifestyle strategies like sleep, hydration, balanced nutrition, light exercise, and stress reduction techniques can help. In persistent or severe cases, consult your doctor.






